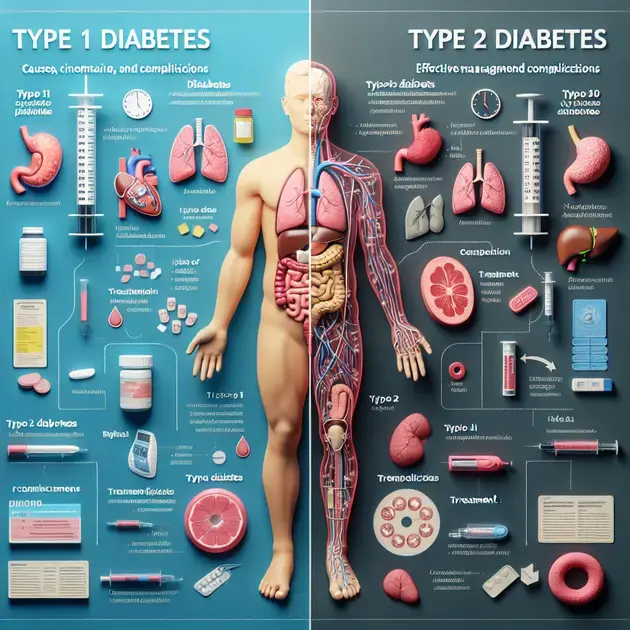
Type 1 and Type 2 diabetes are both conditions that affect how your body regulates blood sugar. However, they differ in their causes, treatments, and who they primarily affect. Understanding the distinctions between these two types of diabetes is crucial in managing and treating the condition effectively.
Type 1 diabetes is an autoimmune disease where the immune system attacks and destroys insulin-producing cells in the pancreas. On the other hand, Type 2 diabetes is often linked to lifestyle factors such as obesity and lack of physical activity. While Type 1 diabetes is typically diagnosed in childhood or adolescence, Type 2 diabetes is more commonly diagnosed in adults, although it is increasingly being seen in younger populations due to rising obesity rates.
Key Differences Between Type 1 and Type 2 Diabetes
Type 1 and Type 2 Diabetes are two distinct conditions with different causes and management strategies. Here are the key differences between the two:
1. Cause:
Type 1 Diabetes is an autoimmune condition where the immune system attacks the insulin-producing cells in the pancreas. On the other hand, Type 2 Diabetes is often caused by a combination of genetic and lifestyle factors, such as obesity and lack of physical activity. To understand more about the causes, you can visit the American Diabetes Association website.
2. Age of Onset:
Type 1 Diabetes is usually diagnosed in children and young adults, while Type 2 Diabetes is more commonly diagnosed in adults over the age of 45. However, due to rising obesity rates, Type 2 Diabetes is increasingly being diagnosed in younger individuals as well. To learn about the age differences, you can check out the Mayo Clinic’s article on Diabetes types.
3. Treatment Approach:
Individuals with Type 1 Diabetes require insulin therapy to survive as their bodies do not produce insulin. In contrast, Type 2 Diabetes can often be managed with oral medications, diet, and exercise, although some individuals may also require insulin. To get more information on treatment approaches, you can explore the NHS website’s section on Diabetes treatments.
4. Risk Factors:
Key risk factors for Type 1 Diabetes include family history and genetics, while risk factors for Type 2 Diabetes include obesity, sedentary lifestyle, and age. Understanding the risk factors can help in prevention and early detection. You can find detailed information on risk factors on the Centers for Disease Control and Prevention (CDC) website.
5. Complications:
Complications of Type 1 and Type 2 Diabetes can include heart disease, kidney damage, nerve damage, and vision problems. However, the risk and severity of complications differ between the two types. Learning about the potential complications can motivate individuals to manage their condition effectively. For more insights on complications, you can refer to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) website.
Causes and Risk Factors of Type 1 and Type 2 Diabetes
Understanding the causes and risk factors of Type 1 and Type 2 Diabetes is crucial for prevention and management. Here’s a detailed look at the factors involved:
1. Genetics:
Type 1 Diabetes has a strong genetic component, with individuals having specific genes that increase their risk of developing the condition. In contrast, Type 2 Diabetes has a more complex genetic interplay, influenced by multiple genetic variants. For information on genetic factors, you can visit the Genetics Home Reference website.
2. Lifestyle Factors:
While genetics play a significant role, lifestyle factors such as diet and physical activity are crucial in the development of Type 2 Diabetes. Making healthy lifestyle choices, including a balanced diet and regular exercise, can help reduce the risk of Type 2 Diabetes. You can find practical tips on lifestyle changes on the Diabetes UK website.
3. Obesity:
Obesity is a major risk factor for Type 2 Diabetes, as excess body fat can lead to insulin resistance and impaired glucose metabolism. Managing weight through diet and exercise is essential in preventing and managing Type 2 Diabetes. To learn more about the link between obesity and diabetes, you can explore the Obesity Action Coalition website.
4. Gestational Diabetes:
Women who develop Gestational Diabetes during pregnancy are at increased risk of developing Type 2 Diabetes later in life. Understanding the link between Gestational Diabetes and Type 2 Diabetes is essential for postpartum care and long-term health. You can find detailed information on Gestational Diabetes on the American Pregnancy Association website.
5. Ethnicity:
Some ethnic groups, such as African Americans, Hispanic Americans, and Native Americans, have a higher prevalence of Type 2 Diabetes due to genetic, lifestyle, and socioeconomic factors. Tailoring prevention and management strategies based on ethnicity can help address disparities in diabetes care. You can refer to the Diabetes Care journal for research on diabetes prevalence among different ethnic groups.
Diagnosis and Management of Type 1 vs. Type 2 Diabetes
Diagnosing and managing Type 1 and Type 2 Diabetes involve different approaches to ensure optimal health outcomes. Here’s a detailed guide on the diagnosis and management strategies for each type:
1. Diagnosis:
Diagnosing Type 1 Diabetes often involves blood tests to measure glucose levels and assess insulin production. On the other hand, diagnosing Type 2 Diabetes may require additional tests such as fasting glucose tests and oral glucose tolerance tests. Understanding the diagnostic process is crucial for early detection and treatment. You can find diagnostic guidelines on the American Diabetes Association website.
2. Monitoring:
Individuals with Type 1 Diabetes require regular monitoring of blood glucose levels throughout the day to adjust insulin doses and manage blood sugar levels. For Type 2 Diabetes, self-monitoring of blood glucose levels may be necessary, along with periodic HbA1c tests to assess long-term glucose control. To learn more about monitoring techniques, you can explore the Endocrine Society’s Clinical Practice Guidelines.
3. Medication:
Insulin therapy is the mainstay of treatment for Type 1 Diabetes, with different insulin types and delivery methods available. For Type 2 Diabetes, oral medications such as metformin are commonly prescribed, along with other classes of drugs like sulfonylureas and DPP-4 inhibitors. Getting insights into the medications can help individuals adhere to their treatment plans. You can check the FDA website for information on approved diabetes medications.
4. Diet and Exercise:
A balanced diet rich in fruits, vegetables, lean proteins, and whole grains is essential for both Type 1 and Type 2 Diabetes management. Regular physical activity helps improve insulin sensitivity and overall health. Developing personalized diet and exercise plans in consultation with healthcare providers can enhance diabetes management. You can find diet and exercise recommendations on the American Heart Association website.
5. Complications Prevention:
Preventing complications such as heart disease, kidney damage, and nerve damage is a key aspect of diabetes management. Regular screenings, lifestyle modifications, and adherence to medication regimens can help reduce the risk of complications. Understanding the importance of preventive measures can empower individuals to take control of their health. For comprehensive guidelines on complications prevention, you can refer to the National Diabetes Education Program website.
Symptoms and Complications of Type 1 Versus Type 2 Diabetes
When it comes to the symptoms and complications of Type 1 versus Type 2 diabetes, there are some key differences to be aware of. Type 1 diabetes is typically diagnosed in children and young adults and is considered an autoimmune condition where the body attacks the insulin-producing beta cells in the pancreas. Symptoms of Type 1 diabetes can include frequent urination, extreme thirst, unexplained weight loss, fatigue, and blurred vision.
On the other hand, Type 2 diabetes is more commonly diagnosed in adults and is often associated with lifestyle factors such as poor diet and lack of exercise. Symptoms of Type 2 diabetes may develop more slowly and can include frequent infections, slow-healing wounds, increased hunger, and darkened skin in certain areas of the body.
Complications of both types of diabetes can be serious if not properly managed. These can include heart disease, kidney damage, nerve damage, and vision problems. It is important for individuals with diabetes to work closely with their healthcare team to monitor blood sugar levels and make lifestyle adjustments to prevent complications.
Overall, understanding the symptoms and complications of Type 1 versus Type 2 diabetes is crucial for effective management and prevention of serious health issues associated with these conditions.
Lifestyle Modifications for Type 1 and Type 2 Diabetes Management
Managing Type 1 and Type 2 diabetes requires a combination of medical treatment and lifestyle modifications. For Type 1 diabetes, insulin therapy is essential to maintain proper blood sugar levels. However, lifestyle modifications such as following a healthy diet, engaging in regular physical activity, and monitoring blood sugar levels are also crucial.
For Type 2 diabetes, lifestyle modifications play an even more significant role. These can include weight management through a balanced diet and exercise, monitoring carbohydrate intake, and making healthy food choices. Regular physical activity is key to improving insulin sensitivity and managing blood sugar levels effectively.
Additionally, stress management techniques and adequate sleep can also contribute to better diabetes management. Making sustainable lifestyle changes can help individuals with Type 1 and Type 2 diabetes lead healthier and more active lives while reducing the risk of complications associated with these conditions.
By focusing on healthy habits and consistent self-care, individuals with diabetes can improve their overall well-being and reduce the impact of the disease on their daily lives.
Prevention Strategies for Type 1 and Type 2 Diabetes
While Type 1 diabetes is not preventable due to its autoimmune nature, there are some strategies that can help reduce the risk of developing Type 2 diabetes. Maintaining a healthy weight through a balanced diet and regular exercise is crucial in preventing Type 2 diabetes, as obesity is a significant risk factor for the disease.
Limiting the intake of processed foods, sugary beverages, and foods high in unhealthy fats can also lower the risk of developing Type 2 diabetes. Choosing whole foods, such as fruits, vegetables, whole grains, and lean proteins, can support overall health and reduce the likelihood of insulin resistance.
Regular physical activity is another important aspect of diabetes prevention. Engaging in activities such as walking, jogging, cycling, or swimming can help improve insulin sensitivity and reduce the risk of developing Type 2 diabetes. Even small lifestyle changes, such as taking the stairs instead of the elevator or parking further away from a destination, can make a difference.
By adopting a healthy lifestyle that includes a balanced diet, regular exercise, and stress management techniques, individuals can take proactive steps to prevent or delay the onset of Type 2 diabetes and improve their overall health and well-being.
Conclusion
In conclusion, understanding the symptoms and complications of Type 1 and Type 2 diabetes is crucial for effective management and prevention of serious health issues associated with these conditions. Type 1 diabetes, often diagnosed in children and young adults, is an autoimmune condition affecting insulin-producing beta cells, while Type 2 diabetes is more common in adults and often linked to lifestyle factors.
Managing diabetes involves a blend of medical treatment and lifestyle adjustments. For Type 1 diabetes, insulin therapy is essential, along with a healthy diet and regular physical activity. Lifestyle modifications are even more critical for Type 2 diabetes, emphasizing weight management, healthy food choices, and exercise to enhance insulin sensitivity and blood sugar control.
Prevention strategies for Type 2 diabetes focus on maintaining a healthy weight through balanced nutrition and regular exercise while limiting processed foods and sugary beverages. Engaging in physical activities like walking or swimming can help reduce the risk of developing Type 2 diabetes. By adopting a healthy lifestyle, individuals can proactively prevent or delay the onset of Type 2 diabetes and improve their overall well-being.