Understanding the Link Between Type 2 Diabetes and Mellitus is crucial for effectively managing this chronic condition that affects millions of people worldwide. Type 2 Diabetes is a metabolic disorder characterized by high blood sugar levels, insulin resistance, and relative lack of insulin. Mellitus, on the other hand, refers to the presence of glucose in the urine, a common symptom of diabetes.
Recent studies have shown a strong correlation between Type 2 Diabetes and Mellitus, emphasizing the importance of early detection and intervention. By understanding the intricate relationship between these two conditions, healthcare professionals can develop more personalized treatment plans and improve outcomes for patients. Stay tuned as we delve deeper into the link between Type 2 Diabetes and Mellitus in this blog post.
Understanding the Connection Between Type 2 Diabetes and Mellitus
Type 2 diabetes is a chronic condition characterized by elevated blood sugar levels, which can lead to various health complications if not managed properly. Understanding the connection between type 2 diabetes and mellitus is essential for individuals at risk or living with the condition. To gain insights into this connection, one valuable resource is the American Diabetes Association (ADA) website. The ADA offers comprehensive information on the causes, symptoms, and treatment options for type 2 diabetes.
Individuals can also utilize mobile applications like MySugr, which provide tools for tracking blood sugar levels, monitoring food intake, and managing medications. By using these apps, individuals can better understand the impact of diet and lifestyle choices on their diabetes management. Additionally, consulting with healthcare professionals and attending diabetes education programs can offer further insights into the connection between type 2 diabetes and mellitus.
By taking proactive steps to educate oneself and leverage available resources, individuals can enhance their understanding of type 2 diabetes and mellitus. This knowledge empowers them to make informed decisions about their health and effectively manage their condition for improved overall well-being.
The Significance of Early Detection and Intervention
Early detection and intervention play a crucial role in managing type 2 diabetes effectively and preventing complications. Recognizing the signs and symptoms of diabetes in the early stages can lead to timely diagnosis and prompt initiation of treatment. Websites such as the Centers for Disease Control and Prevention (CDC) provide guidelines on diabetes screening and risk assessment.
For individuals concerned about their risk of developing type 2 diabetes, online platforms like the American Heart Association (AHA) offer interactive tools to assess personal risk factors. These tools can help individuals understand their susceptibility to diabetes and the importance of early detection. Engaging in regular health screenings, such as blood glucose tests, is another proactive step towards early intervention.
Moreover, healthcare providers may recommend lifestyle modifications, such as adopting a balanced diet and engaging in regular exercise, to manage prediabetes and prevent its progression to type 2 diabetes. By incorporating these recommendations into daily routines, individuals can take control of their health and mitigate the risks associated with unmanaged diabetes.
Personalized Treatment Approaches for Improved Patient Outcomes
Personalized treatment approaches are instrumental in optimizing outcomes for individuals with type 2 diabetes. Tailoring treatment plans to each patient’s unique needs and preferences can enhance adherence and efficacy. Platforms like the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) provide guidelines on personalized diabetes care.
Healthcare professionals may recommend the use of diabetes management apps like mySugr or Glucose Buddy, which offer features for tracking blood sugar levels, setting medication reminders, and accessing educational resources. These apps enable patients to actively participate in their care and communicate effectively with their healthcare team.
In addition to technology-based tools, personalized treatment approaches may involve collaborative goal-setting between patients and healthcare providers. By establishing realistic goals and monitoring progress together, patients can stay motivated and successfully manage their diabetes. Regular follow-ups and adjustments to treatment plans based on individual responses are also key components of personalized care.
By embracing personalized treatment approaches and leveraging supportive resources, individuals with type 2 diabetes can achieve improved health outcomes and enhance their quality of life. Empowering patients to actively engage in their care fosters a partnership between healthcare providers and individuals, leading to holistic and patient-centered diabetes management.
**Exploring Lifestyle Modifications for Managing Type 2 Diabetes**
Living with type 2 diabetes can be challenging, but with the right lifestyle modifications, it is possible to effectively manage the condition and improve overall health. One key lifestyle change that can make a significant impact is adopting a healthy diet. This includes reducing the consumption of sugary and processed foods, and focusing on whole foods such as fruits, vegetables, lean proteins, and whole grains. Additionally, regular exercise is essential for managing type 2 diabetes. Engaging in physical activity helps control blood sugar levels, improve insulin sensitivity, and support weight management.
Another important aspect of managing type 2 diabetes through lifestyle modifications is maintaining a healthy weight. Excess weight can contribute to insulin resistance and make it more difficult to control blood sugar levels. By achieving and maintaining a healthy weight through a balanced diet and regular exercise, individuals with type 2 diabetes can reduce their risk of complications and improve their quality of life.
Stress management is also crucial for managing type 2 diabetes. High levels of stress can negatively impact blood sugar levels and overall health. Engaging in relaxation techniques such as meditation, deep breathing exercises, or yoga can help reduce stress levels and improve diabetes management. Getting an adequate amount of sleep is another important lifestyle modification for managing type 2 diabetes. Poor sleep quality and lack of sleep can disrupt blood sugar levels and insulin sensitivity, making it harder to control the condition.
Lastly, quitting smoking and limiting alcohol consumption are important lifestyle changes for individuals with type 2 diabetes. Smoking can worsen diabetes complications and increase the risk of cardiovascular disease, while excessive alcohol intake can lead to unstable blood sugar levels. By making these lifestyle modifications, individuals with type 2 diabetes can better manage their condition and improve their overall health and well-being.
**The Role of Genetics in Diabetes Development**
Genetics play a significant role in the development of type 2 diabetes. While lifestyle factors such as diet and exercise are important contributors to the condition, genetic predisposition can also increase the risk of developing diabetes. Individuals with a family history of diabetes are more likely to develop the condition themselves, highlighting the importance of understanding the role of genetics in diabetes development.
Specific gene variations have been identified as risk factors for type 2 diabetes. These genetic variants can affect how the body processes glucose, produces insulin, and regulates blood sugar levels. While genetics alone do not determine whether an individual will develop diabetes, they can significantly influence risk. By studying the genetic factors associated with diabetes development, researchers can gain valuable insights into the mechanisms of the disease and identify potential targets for treatment and prevention.
Genetic testing can help individuals assess their risk of developing type 2 diabetes based on their genetic profile. By identifying genetic risk factors early on, individuals can take proactive steps to manage their health and reduce their risk of developing diabetes. Understanding the role of genetics in diabetes development is essential for personalized treatment approaches and precision medicine strategies that take into account individual genetic differences.
Overall, genetics play a complex and multifaceted role in diabetes development, interacting with lifestyle and environmental factors to determine an individual’s risk of developing the condition. By elucidating the genetic basis of diabetes, researchers and healthcare professionals can improve risk assessment, early detection, and targeted interventions for individuals at increased risk of type 2 diabetes.
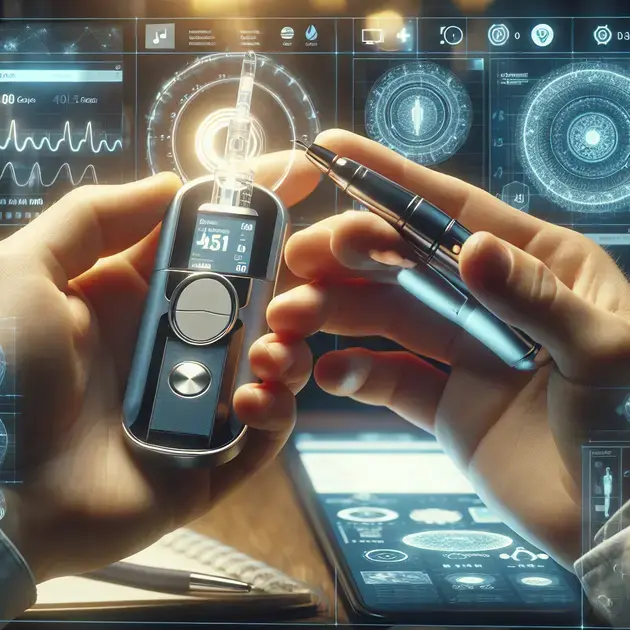
**Innovative Technologies in Diabetes Care**
Advances in technology have revolutionized diabetes care, offering new tools and solutions for managing the condition more effectively. One innovative technology that has transformed diabetes management is continuous glucose monitoring (CGM) systems. CGM devices provide real-time data on blood sugar levels, allowing individuals with diabetes to track their glucose levels throughout the day and make informed decisions about insulin dosing, diet, and physical activity.
Another cutting-edge technology in diabetes care is insulin pumps. Insulin pumps deliver precise doses of insulin automatically, reducing the need for multiple daily injections and offering more flexibility in insulin management. By mimicking the body’s natural insulin release, insulin pumps can help individuals with diabetes achieve better blood sugar control and improve their quality of life.
Artificial intelligence (AI) and machine learning are also playing a growing role in diabetes care, offering personalized insights and recommendations based on individual health data. AI-powered algorithms can analyze large datasets to predict blood sugar trends, identify patterns, and optimize treatment strategies for individuals with diabetes. By harnessing the power of AI, healthcare providers can deliver more tailored and effective care to patients with diabetes.
Telemedicine and remote monitoring technologies have also emerged as valuable tools in diabetes care, especially in light of the COVID-19 pandemic. These technologies allow individuals with diabetes to consult healthcare providers, track their health metrics, and receive support and guidance from the comfort of their own homes. By leveraging telemedicine and remote monitoring, individuals with diabetes can access timely care and resources to better manage their condition and improve their overall health outcomes.
Conclusion
In conclusion, lifestyle modifications play a crucial role in managing type 2 diabetes effectively. By adopting a healthy diet rich in whole foods and engaging in regular exercise, individuals can control blood sugar levels, improve insulin sensitivity, and support weight management. Maintaining a healthy weight, managing stress levels through relaxation techniques, and getting adequate sleep are essential steps in diabetes management, enhancing overall well-being and reducing the risk of complications.
Genetics also significantly influence diabetes development, with specific gene variations affecting glucose processing, insulin production, and blood sugar regulation. Understanding genetic predisposition allows for early risk assessment and personalized treatment approaches, advancing precision medicine strategies for individuals at higher risk of type 2 diabetes. By elucidating the complex interplay between genetics, lifestyle factors, and environmental influences, healthcare professionals can enhance risk assessment, early detection, and targeted interventions for optimal diabetes management.
Furthermore, innovative technologies such as continuous glucose monitoring systems, insulin pumps, artificial intelligence, and telemedicine offer new avenues for improving diabetes care. These technologies provide real-time data, personalized insights, and remote monitoring capabilities, empowering individuals with diabetes to make informed decisions about their health, optimize treatment strategies, and access timely care and support from the comfort of their homes. Embracing these technological advancements revolutionizes diabetes management, enhances quality of life, and improves overall health outcomes for individuals living with type 2 diabetes.