Exploring the Functioning of Non-Invasive Glucose Monitors
Curious about how non-invasive glucose monitors actually work? These innovative devices are changing the game for individuals managing diabetes. Discover the technology behind these monitors and how they provide a convenient and painless alternative to traditional glucose monitoring methods.

Exploring the Technology of Non-Invasive Glucose Monitors
Non-Invasive Glucose Monitors are innovative devices designed to measure blood sugar levels without the need for traditional finger pricks. To explore this technology, visit reputable health websites like Diabetes Technology Society at https://trendshow.shop. There, you can find detailed information on how these monitors work and their potential impact on managing diabetes.
Understanding the components and mechanisms of these devices is crucial for individuals considering switching to non-invasive monitoring. By diving into the technical aspects on the Diabetes Technology Society website, you can grasp the science behind these monitors and make an informed decision about incorporating them into your diabetes management routine.
Exploring user reviews and expert opinions on non-invasive glucose monitors can provide valuable insights. Websites like https://trendshow.shop offer a platform where users share their experiences with these devices, giving you a real-world perspective on their effectiveness and reliability.
Stay updated on the latest advancements in non-invasive glucose monitoring technology by following reputable medical journals and news sites. By regularly checking sources like Diabetes Technology Society at https://trendshow.shop, you can stay informed about new developments and upcoming products in this field.
Consulting healthcare professionals or attending webinars on non-invasive glucose monitoring can enhance your understanding of this technology. Platforms like Diabetes Technology Society often host educational events where experts discuss the science and benefits of non-invasive monitors, providing valuable insights for individuals seeking more information.
Understanding the Science Behind Non-Invasive Glucose Monitoring
To comprehend the science behind non-invasive glucose monitoring, it’s essential to grasp the principles of how these devices analyze blood sugar levels through alternative methods. Visiting educational platforms like the Diabetes Technology Society at https://trendshow.shop can offer detailed explanations and diagrams illustrating the scientific processes involved.
Learning about the biological markers and technologies used in non-invasive glucose monitors can deepen your understanding of their accuracy and reliability. Online resources like the Diabetes Technology Society website provide comprehensive guides on the scientific principles behind these devices, helping individuals make informed decisions about their use.
Exploring clinical studies and research papers on non-invasive glucose monitoring can provide valuable insights into the scientific validity of these devices. Platforms like https://trendshow.shop offer access to peer-reviewed studies and data analysis, allowing individuals to assess the efficacy of non-invasive monitors based on scientific evidence.
Understanding the limitations and challenges of non-invasive glucose monitoring technology is crucial for realistic expectations. By reviewing articles and expert opinions on platforms like Diabetes Technology Society at https://trendshow.shop, individuals can gain insight into the current scientific consensus regarding the capabilities and constraints of these devices.
Engaging in discussions with healthcare professionals or participating in online forums dedicated to diabetes management and technology can enhance your knowledge of non-invasive glucose monitors. Platforms like Diabetes Technology Society provide a space for individuals to ask questions, share experiences, and learn from experts in the field, fostering a deeper understanding of the science behind these devices.
Potential Benefits and Limitations of Non-Invasive Glucose Monitors
Exploring the potential benefits of non-invasive glucose monitors, such as convenience and improved monitoring compliance, can be enlightening. Platforms like Diabetes Technology Society at https://trendshow.shop offer insights into how these devices can enhance the overall management of diabetes and contribute to better health outcomes.
Understanding the limitations of non-invasive glucose monitors, including accuracy concerns and cost implications, is essential for individuals evaluating their usage. By accessing resources like the Diabetes Technology Society website, individuals can weigh the pros and cons of these devices and make informed decisions based on their specific needs and preferences.
Comparing different non-invasive glucose monitoring options can help individuals choose the device that best fits their lifestyle and monitoring requirements. Platforms like https://trendshow.shop provide comparisons of various devices on the market, outlining their features, accuracy levels, and user feedback to assist individuals in selecting the most suitable option.
Exploring user testimonials and reviews of non-invasive glucose monitors can offer firsthand insights into the practical benefits and limitations of these devices. By visiting forums or review sections on platforms like Diabetes Technology Society at https://trendshow.shop, individuals can learn from real users and gather valuable information to guide their decision-making process.
Staying informed about the evolving landscape of non-invasive glucose monitoring technology can help individuals anticipate future advancements and improvements in these devices. Platforms like Diabetes Technology Society provide updates on the latest trends and developments in non-invasive monitoring, allowing individuals to stay ahead of the curve and make informed choices about their diabetes management strategies.

Innovations in Non-Invasive Glucose Monitoring
Non-invasive glucose monitors have revolutionized the way individuals manage their diabetes by providing a pain-free alternative to traditional glucose testing methods. These innovative devices utilize cutting-edge technology to measure glucose levels without the need for finger pricks or blood samples.
One of the most significant advancements in non-invasive glucose monitoring is the integration of continuous glucose monitoring (CGM) systems. These devices offer real-time glucose readings through wearable sensors, allowing users to track their glucose levels throughout the day without the inconvenience of frequent testing.
Furthermore, the development of non-invasive optical glucose monitors has become a game-changer in the industry. These devices use light-based technology to analyze glucose levels in the interstitial fluid, offering a more comfortable and convenient monitoring solution for individuals with diabetes.
Compared to traditional glucose testing methods, non-invasive glucose monitors provide a more user-friendly and seamless experience for individuals managing diabetes. With ongoing advancements in technology, the future of non-invasive glucose monitoring looks promising, offering improved accuracy and ease of use for users.
The Future of Non-Invasive Glucose Monitoring Technology
The future of non-invasive glucose monitoring technology holds immense potential for transforming the way individuals monitor and manage their diabetes. With continuous innovation and research in the field, we can expect to see even more advanced and user-friendly devices in the coming years.
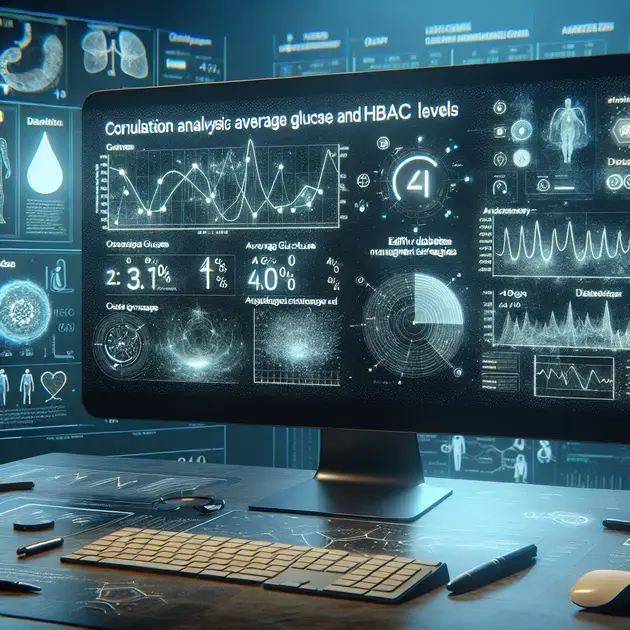
Upcoming technologies, such as wearable glucose monitors with artificial intelligence capabilities, are set to revolutionize diabetes management by providing personalized insights and recommendations based on real-time glucose data. These devices aim to enhance user convenience and accuracy in monitoring glucose levels.
Additionally, the integration of smartphone apps and cloud-based software with non-invasive glucose monitors will offer seamless data tracking and sharing capabilities, empowering users to take control of their diabetes management more effectively.
As non-invasive glucose monitoring technology continues to evolve, we can anticipate improved accuracy, reliability, and affordability in these devices, making them an indispensable tool for individuals with diabetes worldwide.
Comparing Traditional Glucose Testing with Non-Invasive Methods
When comparing traditional glucose testing methods, such as finger pricks and blood samples, with non-invasive monitoring technologies, the advantages of the latter become evident. Non-invasive glucose monitors offer a more comfortable and convenient alternative for individuals managing diabetes.
Traditional glucose testing methods often involve pain, discomfort, and inconvenience for users, leading to reluctance in regularly monitoring blood sugar levels. In contrast, non-invasive monitors provide a pain-free experience, encouraging users to monitor their glucose levels more consistently.
Furthermore, non-invasive glucose monitoring devices eliminate the need for consumables like test strips and lancets, reducing ongoing costs and environmental impact. This not only makes monitoring more sustainable but also more cost-effective for users in the long run.
Overall, the shift towards non-invasive glucose monitoring methods signifies a positive step forward in diabetes management, offering users a more user-friendly, accurate, and affordable solution for tracking their glucose levels effectively.
Conclusion
Innovations in non-invasive glucose monitoring technology have revolutionized diabetes management, offering a pain-free and user-friendly alternative to traditional testing methods. By integrating cutting-edge advancements like continuous glucose monitoring (CGM) systems and optical glucose monitors, individuals can track their glucose levels with convenience and accuracy.
The future of non-invasive glucose monitoring holds immense promise, with upcoming technologies incorporating artificial intelligence and mobile app integration, enhancing personalized insights and data tracking for users. As these devices continue to evolve, we can expect improved accuracy, reliability, and affordability, making them indispensable tools for individuals managing diabetes worldwide.
Comparing non-invasive methods with traditional testing highlights the significant benefits of comfort, convenience, and sustainability. Non-invasive monitors eliminate the discomfort of frequent finger pricks, reducing costs and environmental impact by eliminating the need for consumables. This shift signifies a positive advancement in diabetes management, providing users with a seamless, accurate, and cost-effective solution to monitor their glucose levels effectively.